INTRODUCTION
Chemotherapy-induced peripheral neuropathy (CIPN) is a dysesthesia or pain of peripheral nerve caused by anticancer drugs during chemotherapy. It varies with the kind of chemotherapy agents but CIPN occurs with a relatively high frequency and substantially decreases quality of life. It limits a dose of chemotherapy and even interferes the regular schedule of chemotherapy potentially [1–3]. Many patients with chemotherapy experience mild CIPN in their hands and feet during the early stages of chemotherapy and complain of tingling sensations in their palms and soles and pain or pinching sensation in the fingers and toes. It has been reported that even grade-2 CIPN can have a significant impact on patients’ quality of life [2]. Although the symptoms of CIPN are alleviated by stopping treatment, adjusting doses, or are relieved with time, they may persist until after the end of treatment [1,2]. The most significant problem is that preventive or therapeutic measures for CIPN have not been clearly established yet [1,2,4,5]. As there is no definite and effective treatment for CIPN, interest in “alternative therapy” has been increasing. In particular, an attempt to demonstrate the effectiveness of manual therapy, such as rehabilitation programs to stimulate the muscles of the hands and feet, have been made. Because we believe that rehabilitation program using minor hand muscles is a valuable alternative therapy in alleviating the symptoms of neuropathy, we tried to apply this program to patients with CIPN symptoms. Also, in order to suggest symptom-targeted treatments for CIPN, it is necessary to have an appropriate understanding of symptoms that many patients actually complain about. Then, we can develop treatments that can be accepted by CIPN patients based on those appropriate understanding.
The purpose of this study is to identify common symptoms of CIPN and to verify the efficacy of the rehabilitation program.
METHODS
Patients
The basic handicrafts program was performed for patients who were diagnosed with colorectal cancer in this hospital and were being followed up with chemotherapy after surgical treatment. In the recruitment process, voluntary participation was encouraged without limiting it by the location of tumors, cancer stages, operation types or chemotherapy regimens. However, the patients who had diabetes mellitus or neurologic diseases, which could affect neuropathic symptoms, were excluded. Although 16 patients participated in this handicrafts program, 11 patients were finally included in the study after the participation of the program and submission of questionnaires.
Chemotherapy regimens
The chemotherapy regimens used in this study were “5-fluorouracil (5-FU) with leucovorin (LV),” “combination with infusional 5-FU, LV and oxaliplatin (FOLFOX4),” and “combination with infusional 5-FU, LV and irinotecan (FOLFIRI).” The detailed regimen is as follows.
Patients who were treated with 5-FU and LV received 20 mg/m2 of LV and 400 mg/m2 of 5-FU for 5 days at an interval of 4 weeks. Patients who used FOLFOX4 regimen received 85 mg/m2 of oxaliplatin and 400 mg/m2 of 5-FU (bolus), then followed by 600 mg/m2 of 5-FU via infusion with LV for 2 days. It was performed every 3 weeks. Patients who were treated with the FOLFIRI regimen received 150 mg/m2 of irinotecan and 400 mg/m2 of 5-FU (bolus), and then followed by 600 mg/m2 of 5-FU for 2 days via infusion with LV with an interval of 3 weeks.
Rehabilitation program (the basic handicrafts program)
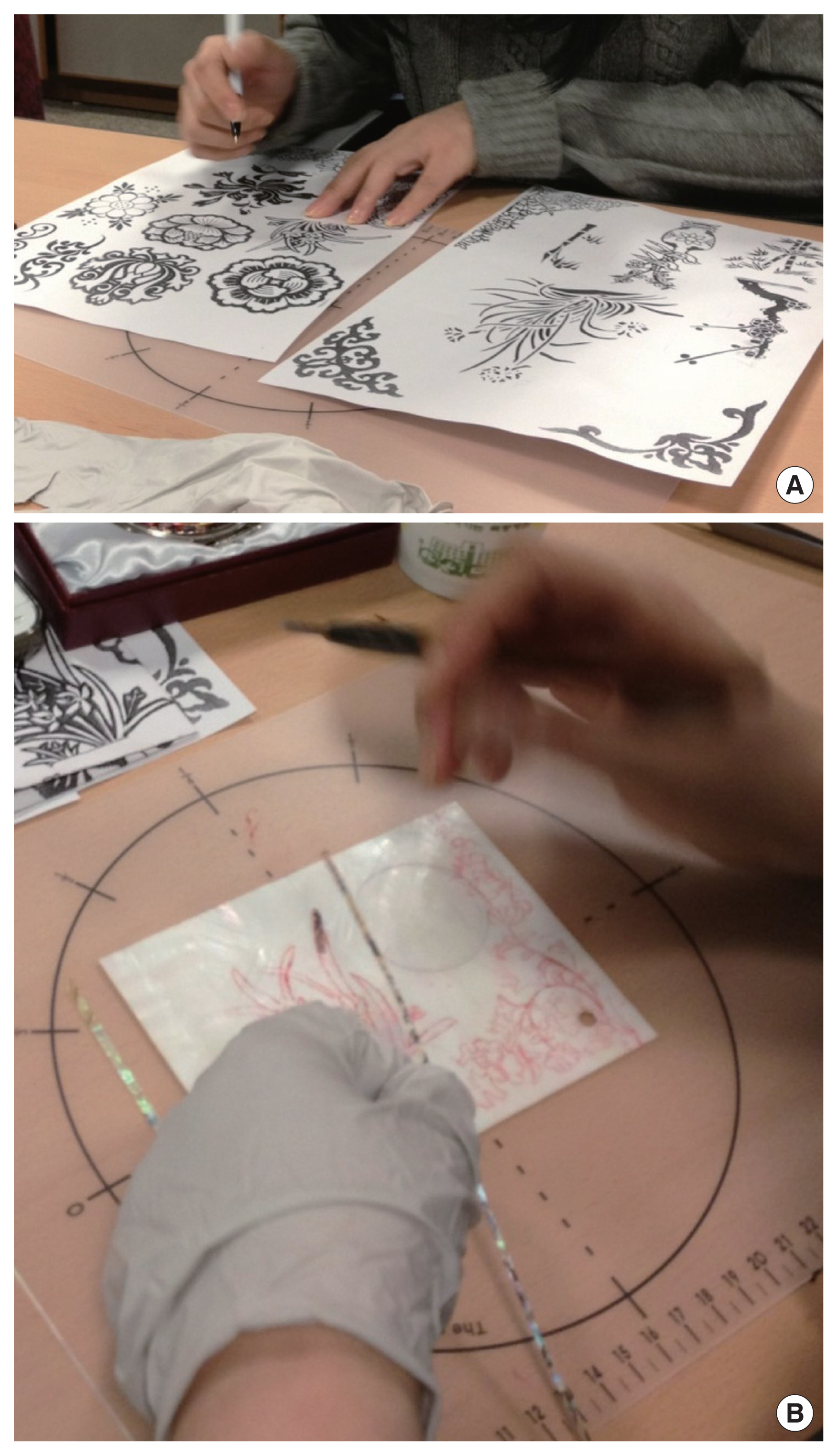
The aim of this program is to promote using the minor muscles of the hands by decorating handicrafts such as a hand mirror, a business card holder, a table clock, and a picture frame with lacquerware, using the Korean traditional lacquerworks (Fig. 1). The process to make lacquerworks in this handicraft class was as follows. First, participants designed his/her craft, then cut the lacquerware into various sizes and shapes according to the design. The more complicated the sizes or shapes of design was, more scrupulous and careful attention was required to handle the lacquerware (Fig. 2). Prepared lacquerware was attached on the appropriate locations of hand mirror, a business card holder, a table clock, and a picture frame using glue.
This was performed once a week, for 2 hours per session, for a total of 4 weeks through outpatient clinics. The program was conducted under the supervision of not only a professional instructor but also specialized nurses and a surgeon.
Questionnaire and data collection
The questionnaire used in this study is based on a revised short-form McGill Pain Questionnaire (SF-MPQ-2) [6]. This questionnaire is designed to evaluate the characteristics of neuropathic pain; a responder is supposed to directly measure the degree of his/her pain by setting the score of 0 for no specific neuropathic pain and 10 for the worst pain. On an 11-point scale, the range of the score is from 0 to 220 on the 22-item questionnaire. In a previous study [7], the content validity of Korean Short-form McGill Pain Questionnaire (SF-MPQ) was verified as the content validity indices of 0.53–0.80 and the alpha coefficient was 0.86. We modified the Korean SF-MPQ to suit SF-MPQ-2 and used it in this study.
The questionnaire was collected by specialized nurses before the beginning of handicraft class and after the completion of the 4th class. This study was approved by the Institutional Review Board (IRB) of Ewha Womans University Mokdong Hospital (IRB No. EUMC 2018-03-029-002). The requirement of informed consent was waived by IRB.
Statistical analysis
Statistical analysis was performed using IBM SPSS version 20.0 (IBM Corp., Armonk, NY, USA). The measurement data such as age or scale score were expressed as mean±standard deviation. The Korean SF-MPQ-2 score before and after participation in the program was analyzed using a paired t-test. Statistical significance was defined when the significance level (P-value) was less than 0.05.
RESULTS
Among 16 patients who participated in the program, 11 finished the rehabilitation program without dropping out, responded to a questionnaire, and were finally included in this study. Among these, there were three men and eight women. Their mean age was 53.0±11.2 years old. The mean body mass index was 23.4±5.7 kg/m2 (Table 1). Two patients were taking antihypertensive drugs due to their hypertension, and one patient was being followed up due to bronchiectasis. One patient was diagnosed with breast cancer in other hospital and surgically treated in 2010, then she was being followed up without chemotherapy.
One of the patients underwent laparoscopic right hemicolectomy for ascending colon cancer, and two patients underwent laparoscopic anterior resection for sigmoid colon cancer. Eight patients had rectal cancer; among these, one patient underwent laparoscopic low anterior resection, one patient underwent hand-assisted laparoscopic low anterior resection, five patients had low anterior resection, and the other patient had abdominoperineal resection. Based on the final pathology, three patients were stage I, one patient was stage II, and seven patients were stage III (American Joint Committee on Cancer staging 7th edition) (Table 1).
Six of 11 patients underwent radiation therapy before and after surgery. Six of 11 patients received 5-FU chemotherapy, and four patients received a FOLFOX4 regimen. One patient received 5-FU, followed by FOLFIRI and FOLFOX4 chemotherapy, in that order, after surgery. Patients underwent 9.7±8.9 cycles of chemotherapy on average (Table 1).
The mean number of the rehabilitation programs that these patients participated in was 3.8±0.4. The mean score on the Korean SF-MPQ-2 was 34.1±31.7 in pre-program, and 24.4±21.5 in post-program, showing a significant difference in the results of the questionnaire before and after the rehabilitation program (P=0.040) (Table 2, Fig. 3). Also, among a total of 22 symptoms in the questionnaire, the common symptoms found in more than 80% of the entire patients were 12 symptoms including throbbing pain, shooting pain, stabbing pain, aching pain, heavy pain, tender pain, tiring-exhausting, fearfulness, punishing cruel, itching, tingling or “pins and needles,” and numbness. The most common CIPN symptoms among these were shooting pain and tingling or “pins and needles.” In particular, tingling or “pins and needles” sensations showed a statistically significant difference before and after the program participation (P=0.038) (Table 2).
DISCUSSION
The incidence of CIPN is relatively as high as 60% to 70% [2,8–10], although it varies depending on the type of anticancer agents or regimens and administered methods [11–13]. In this study, the incidence of CIPN was 81.8% (9/11) and it was not related with chemotherapy regimens or dosage either (P=0.564 and P=0.186).
The mechanism of neuronal damage in CIPN is not fully understood [14,15]; therefore, there are no firmly established preventions or therapies and the researches to understand CIPN and to find its treatment is continuing [4,5,16]. Even the drugs used for CIPN treatments nowadays, such as tricyclic antidepressants, gabapentin, lamotrigine, topical baclofen amitriptyline and ketamine, have not been sufficiently proven in effect of pain relief [16]. Because of the disappointing results of pharmacotherapeutics, the interest in alternative treatment is increasing. Researchers attempt to approach the neuropathic pain through the symptom-targeted therapies. Some recent studies have focused on neuropathic pain and are paying attention to treatments that target symptoms themselves. The behavioral technique, physical exercise, and manual therapy are all alternative treatments; however, the effect is not proven yet evidently [1,4,5].
In particular, manual therapy, which is also called therapeutic massage, had been reported in previous studies to reduce neuropathic symptoms [2]. Also, one of the important advantages of manual therapy is that the patient can take the initiative in accordance with their own behavior [3], and thus the compliance with the treatment is expected to be very high. The mechanism by which the manual therapy affects CIPN is not completely known. Manual therapies cause changes in blood circulation including changes in the blood flow and temperature of extremities as shown by thermography. The temperature changes that CIPN patients experience through manual therapy is related to the improvement of symptoms such as tingling sensations, numbness, and pain. Although the association between blood flow and CIPN symptoms is not well known, it is supposed that the improved blood flow affects the effective supply of nutrients as well as oxygen, and promotes the recovery by removing residual neurotoxic substances of chemotherapy [2].
The modified manual therapy for CIPN suggested in this study is a well-organized rehabilitation program using minor muscles. Instead of merely receiving massage passively, the patients were able to use the minor muscle actively through the craftwork. We tried to improve symptoms by stimulating the muscles by combining massage and physical exercise. Its noticeable advantage is patients can readily follow the process and need to use minor muscles of the hands, which are usually not used. Because CIPN often occurs in the palm or fingers and can cause functional disability in a severe case, it is very significant to improve blood circulation by stimulating the hand muscles through this rehabilitation program.
In fact, the degree of neuropathic symptoms that patients experienced before and after the rehabilitation program through a handicraft class provided by this hospital significantly decreased from 34.1 to 24.4 (P=0.040). Although the degree of tingling sensations among the detailed items was not severe, there was a significant difference before and after the program (P=0.038) (Table 2).
Moreover, because the participants in the rehabilitation program were patients undergoing similar anticancer treatments, this program propelled discussions among patients with similar symptoms to share and relieve anxiety. As a result, their concentration increased while performing a delicate task during handicrafts preparation. An exhibition and rummage sale (Fig. 2B) was held for dispersing pearl handicrafts made by the participants during the handicraft class. This was expected to increase the activeness and confidence of patients. The evaluation items of the Korean SF-MPQ-2 used in this study included not only questions regarding peripheral neuropathy but also emotional aspects. We expected that those emotional symptoms would also improve; however, these factors did not show significant results (punishing cruel: pre-program score 2.2±4.0 points, post-program score 1.1±3.0 points, P=0.258; fearfulness: pre-program score 2.6±3.9 points, post-program score 2.4±3.9 points, P=0.659) (Table 2). In case that a study is performed in a larger patient group in the future, it would be essential to analyze outcomes focusing on the emotional support effect of this program.
The limitations of this study are as follows. First, the number of patients included in the study was not sufficient to definitively prove the efficacy of the program. For a small number of patients who could be recruited and enrolled within the limited resources at the time that this rehabilitation program was planned, this study was performed as a pilot study to identify the effect of the rehabilitation program for CIPN. Additionally, considering that the symptoms and degree of CIPN vary from person to person and can be different depending on the type of chemotherapy, the difference was developed based on the type of chemotherapy even before participating in the program because the types of chemotherapy of 11 patients were not controlled. This needs to be complemented through a larger study, and the effect of the rehabilitation program according to the type of chemotherapy needs to be investigated. Moreover, the period of conducting the program was relatively short to properly evaluate the effect of the rehabilitation program. The period of chemotherapy varies from 6 months to 12 months or more according to the type of regimen. Also, it is a limitation of this study that there is a lack of objective indicators to verify the improvement of blood circulation, like by using Doppler ultrasound or by measuring the temperature of a hand before and after the program, in addition to the questionnaire to examine the improvement of symptoms that patients subjectively experience. Therefore, it is necessary to recruit a greater number of patients and to conduct an additional study with long-term follow-up.
If a dramatic effect cannot be expected with the known pharmacologic therapy for CIPN treatment, it is necessary to study and establish a symptom-targeted alternative therapy. This study paid attention to manual therapy. Rehabilitation using the minor muscles of hands alleviates CIPN symptoms significantly. Therefore, it is essential to verify the effect of a rehabilitation program in CIPN treatment.