INTRODUCTION
Laparoscopic liver resection (LLR) has been very common due to the development of techniques and medical devices since 1992. In 2008, experts in liver surgery established the “Louisville Statement,” a set of guidelines about the rapidly growing area of minimally invasive liver resection. The number of LLRs reported has consistently increased, especially since 2009. Although minor LLRs have been performed usually in clinical practice, reports of major and anatomic LLRs have increased sharply [1,2]. Some specialized centers have reported favorable and competitive outcomes of LLR compared to open liver resection (OLR). Liver cancer lesions located in the right upper lobe of the liver or invading the diaphragm are difficult subjects for LLR. Moreover, in the case of a patient with cirrhosis of Child B and mild ascites, hepatic resection of segment 7 or 8 is more difficult. In this case, LLR unnecessarily removes a large amount of liver parenchyma, reducing the remnant liver volume and also OLR may cause damage to the abdominal wall and cavernous reticulum, resulting in more severe cirrhosis and ascites, and eventually liver failure.
In patients with marginal liver function, no further radiofrequency treatment or trans-arterial chemoembolization (TACE) was possible, and LLR or OLR was not possible. Hepatectomy was attempted through video-assisted transthoracic liver resection (VTLR). We report a case of liver resection using the modified Kelly fracture method using Harmonic Scalpel (Ethicon Endo-Surgery, Inc., Cincinnati, OH, USA) ultrasonic shears.
METHODS
All of the procedures were in accordance with the ethical standards of the responsible committees on human experimentation (institutional and national ) and with the 1964 Declaration of Helsinki and later versions. This study was approved by the Institutional Review Board of Hallym University Sacred Hospital (registration number: HALLYM 2020-11-003). Between March 2017 and February 2020, patients who underwent VTLR were collected retrospectively from a prospectively established database.
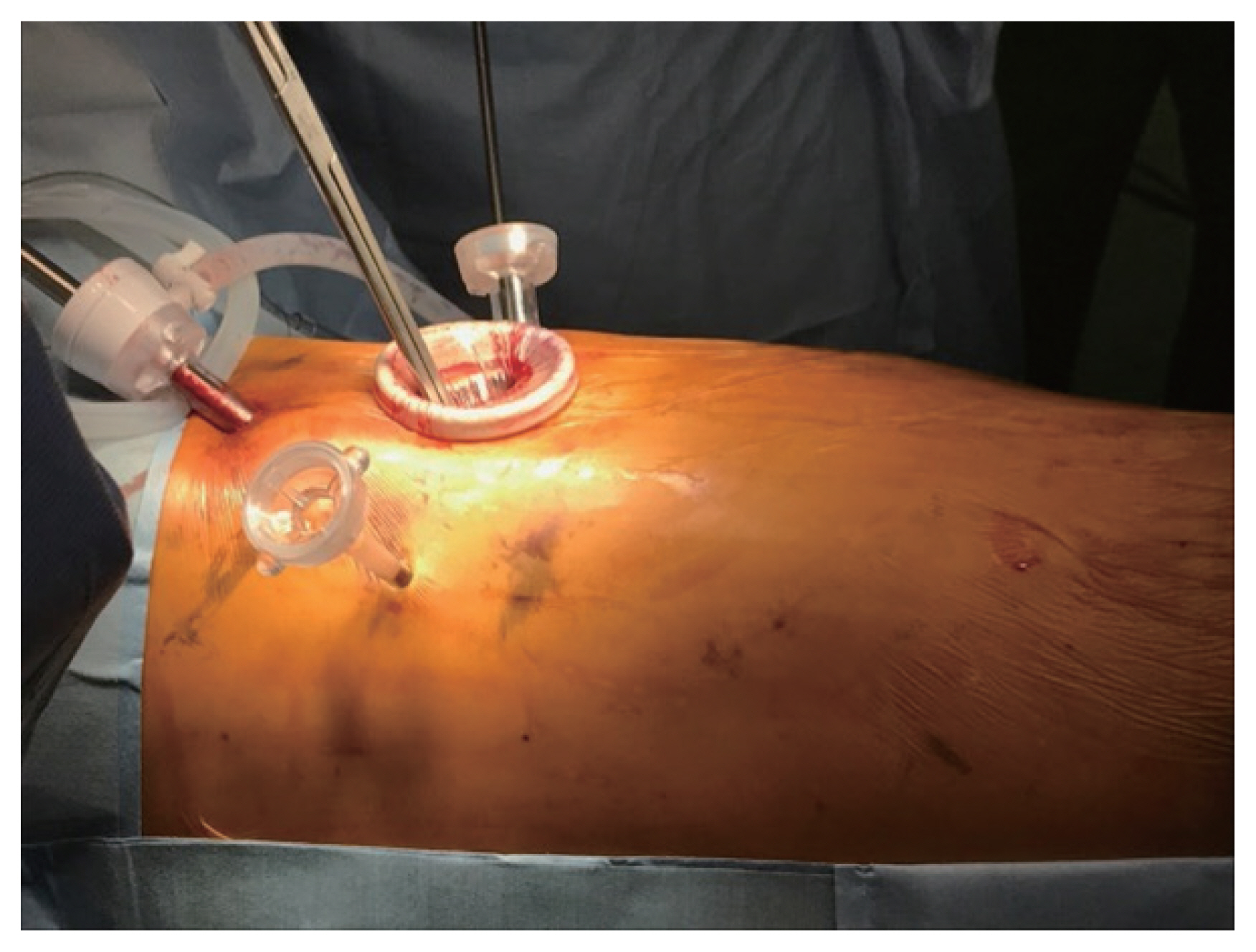
In the cases with moderate liver cirrhosis, radiofrequency ablation, and TACE were not possible due to severe cirrhosis, marginal liver function, or diaphragm invasion, liver resection could be achieved through thoracoscopic approach. The patient was placed left lateral decubitus position with the surgeon standing behind of the patient (Fig. 1). One lung ventilation was required under general anesthesia to perform VTLR. After the injection of sodium fluorescein, the diaphragm adjacent to the area of the sodium fluorescein enhanced lesion visible through the diaphragm was incised, and Vicryl 3-0 (Ethicon Endo-Surgery, Inc.) traction tagging was performed in 3 to 4 places. Additionally, the surgeon identified the location of the lesion and the boundary of the segment using intraoperative ultrasound, then marked the lesion using a monopolar coagulator, and cuts the hepatic parenchyma using the Kelly fracture method with Harmonic Scalpel (Ethicon Endo-Surgery, Inc.) ultrasonic shears. The Glissonean pedicle and hepatic vein is seen on intraoperative ultrasound should be ligated using a metal clip if possible (Fig. 2).
RESULTS
This study included three hepatocellular carcinoma patients and one metastatic liver malignancy from colon cancer who underwent VTLR from March 2017 to February 2020. Their mean age was 52.3 years (range, 49–63 years). The underlying liver disease was hepatitis B virus in three patients (75%) and drug-induced hepatitis in one patient (25%). The mean indocyanine green retention rate at 15 minutes (ICG 15) of the patient group was 12.3% (range, 9%–15%). Preoperative serum international normalized ratio, total bilirubin, and albumin results were 1.02 (range, 0.8–1.3), 1.03 mg/dL (range, 0.8–1.3 mg/dL), and 3.64 g/dL (range, 3.3–4.2 g/dL), respectively. According to the Child-Pugh classification, three patients (75%) belonged to class A, and one (25%) was placed in class B. On average, patients started to consume a normal diet on the average of 2.4 days (range, 1–4 days), and were discharged after an average of 11.3 days (range, 6–15 days) of hospitalization. VTLR was carried out in segment 7 in two cases and in segment 8 in two cases (Table 1).
DISCUSSION
LLR has been continuously developing since 2008. Laparoscopic resection of tumors located in the left lobe or superficial hepatic lobe is relatively easy. In the case of a tumor that is biased to the right, resection is relatively easy. However, laparoscopic resection of tumors located in the posterior segment, especially in the right upper lobe that invades the diaphragm, is difficult. This is a study to evaluation the technique of performing VTLR for liver malignancy located in right upper area with marginal liver function.
Several studies have shown the usefulness of thoracoscopic liver resection. Excessive bleeding is a major problem in cirrhotic liver resection, and many studies have used coagulation techniques such as microwave tissue coagulation, TissueLink monopolar sealer, or radiofrequency waves [3,4]. In this study, ultrasound was performed before incision of the diaphragm to determine the location of the liver lesion, and thoracoscopic liver resection was performed using the Kelly fracture method using an ultrasonic cutting machine rather than the radiofrequency ablation method. An ultrasonic cutting machine made an incision space for the liver parenchyma through ultrasonic cavitation, and the exposed Glissonean pedicle and hepatic vein were ligated with clips.
In determining the location of the sub-diaphragm tumor, in this study, the location was determined using intraoperative ultrasound before incision of the diaphragm. Recently, intervention-guided fluorescence imaging technique or indocyanine green under infrared light methods to confirm the location of liver tumors are also expected to be utilized [5].
Hepatic resection has been proven to be an effective treatment modality for the treatment of hepatocellular carcinoma and metastatic colorectal cancer [6]. In this study, patients with marginal liver function in the upper right liver segment did not have an accessible hepatic artery through frequent TACE, so TACE was no longer possible. It shows that hepatic resection can be performed by maximally preserving the remaining liver parenchyma through VTLR and securing minimal surgical margin.