Clinicopathologic characteristics of teenage sporadic colorectal cancer
Article information
Abstract
Purpose
Colorectal cancer (CRC) is generally considered a disease of old age. Most CRCs are diagnosed at age 50 and over. CRC rarely occurs in teenagers, and the clinical features and prognosis of CRC are not clear in this population. The aim of this study was to uncover the clinicopathologic characteristics of teenage sporadic CRC.
Methods
Of the 21,042 patients who underwent operation for primary CRC at Asan Medical Center between July 1989 and December 2014, 19 cases (0.09%) without a familial history of CRC before 20 years of age at diagnosis were enrolled in this study. The clinicopathologic features of the teenage sporadic CRC patients were retrospectively reviewed.
Results
Of the 19 patients, 16 patients (84.2%) were male. The most common primary site was the left colon (descending colon & sigmoid colon) in nine patients. With respect to histologic type, adenocarcinoma represented 57.8% of cases, mucinous adenocarcinoma, 31.5%, and signet ring cell carcinoma, 10.5%. Six (31.5%) patients showed peritoneal seeding at presentation. In survival analysis, the 5-year overall survival rate of the patients who underwent curative surgery was 71.3%.
Conclusion
Teenage sporadic CRC is a very rare disease and the proportion of patients with a poor histologic subtype is high, but early detection and radical treatment can lead to favorable survival rates.
INTRODUCTION
Colorectal cancer (CRC) is the third most common cancer among Koreans and the fourth leading cause of death in Korea [1]. The risk factors of CRC include old age, obesity, race, family history, and smoking. With respect to age, 90% of all CRC cases were found in patients aged over 50 years [2–5]. In general, it is believed that CRC occurs more frequently in older people. It is, however, possible that sporadic CRC can occur in teenagers, albeit quite rarely, even when they have no family history of CRC. A CRC incidence rate of 0.3–1.5 per million teenagers has been reported [6]. Given the low incidence of CRC, the clinicopathological characteristics of sporadic CRC in young people have not been well documented. The current study therefore aimed to investigate the clinicopathological significance and prognosis of sporadic CRC in young people who underwent CRC surgery before the age of 20.
METHODS
This retrospective study was conducted to investigate clinicopathological features in young patients under 20 years of age who were selected from 21,042 CRC patients who underwent surgery in the Colorectal Department of Asan Medical Center in Seoul from July 1989 to December 2014. The diagnosis of a CRC lesion was confirmed by a histopathological exam before surgery in the target group. We excluded a case of lymphoma and 4 cases of colonoscopy-detected familial adenomatous polyposis plus a family history. A total of 19 (0.09%, 19/21,042) sporadic CRC patients under age 20 met the inclusion criteria. We retrospectively analyzed patient data including sex, primary tumor location, histological subtype, carcinoembryonic antigen levels, surgical technique, and pathological stage using the database of CRC patients and consequent outcomes such as relapse and mortality during follow-up. Prognosis assessment was performed based on survival analysis using the Kaplan-Meier method.
The primary tumor location was classified into ascending colon, transverse colon, descending colon, sigmoid colon, and rectum (upper, middle, and lower). CRC is histologically divided into 3 categories: adenocarcinoma, mucinous adenocarcinoma, and signet ring cell type. Both conservative and radical surgical treatments were used, and the patients were classified into TNM stages based on postoperative histopathological results. The follow-up period included a final outpatient visit made after surgery, and the mean follow-up period was 68.9 months.
RESULTS
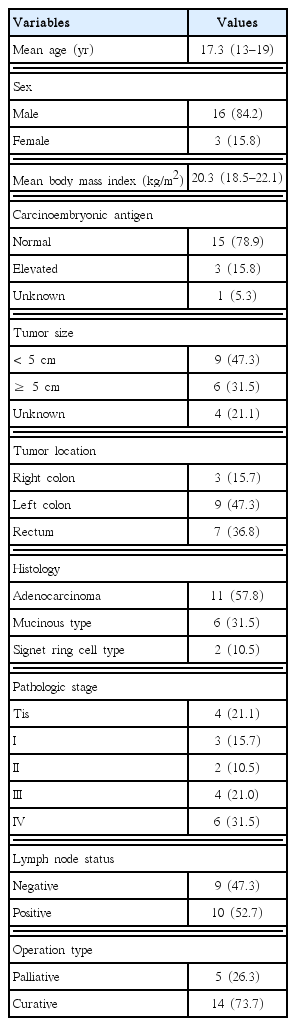
There were 16 male patients (84.2%) and 3 female patients (15.8%) with an overall mean age of 17.3 years (range, 13–19 years) at the time of diagnosis. The clinicopathological characteristics of the patients are summarized in Table 1. The lesions were present in the right colon (the ascending and transverse colons) in 3 cases (15.7%), in the left colon (the descending colon) in 9 cases (47.3%), and in the rectum in 7 cases (36.8%). In terms of histological subtype, adenocarcinoma was identified in 11 cases (57.8%), mucinous adenocarcinoma in 6 cases (31.5%), and signet ring cell type in 2 cases (10.5%). Of 19 patients, 10 (52.5%) progressed to stages III–IV at the time of surgery (4 cases of stage III and 6 cases of stage IV), and peritoneal metastasis was detected during surgery in the stage IV group. Fourteen patients (73.7%), including 1 patient with partial peritoneal metastasis, were suitable for radical surgery. The clinicopathological characteristics of 19 individual patients are presented in Table 2.
Although the patients for whom only conservative means were allowed had a 1-year survival rate of 20%, the patients who underwent radical surgery showed a 5-year survival rate of 71.3% (Fig. 1).
DISCUSSION
A higher incidence of CRC was observed in male teenagers (16/19, 84.2%) in this study. Although only 3 cases of CRC were found in female teenagers, they had a severe outcome with an average survival period of 12 months: two of them developed peritoneal metastasis and one had a tumor that spread to the renal fascia as a stage IIIc cancer. Continued studies with larger sample sizes are needed to verify why the incidence of CRC is higher in male teens than female teens and why the latter group had aggressive outcomes.
Researchers are divided in their views regarding the most common site of the first lesion in sporadic CRC among young patients: Some of them reported that CRC was most often located in the ascending colon [7,8], whereas others noted the descending colon or rectum as the most common location, which is the same for adult patients [9]. In the present study, the descending colon or rectum was the most frequent location (16/19, 84.2%). Regarding histological subtype, adenocarcinoma is the most common type, being found in 85% of adult CRC patients, followed by mucinous adenocarcinoma (10%–15%) and signet ring cell type (1%) [10]. Unlike CRC in adults patients, however, in young patients, the most common types were mucinous adenocarcinoma (6/19, 31.5%) and signet ring cell type (2/19, 10.5%). Normally, mucinous adenocarcinoma and signet ring cell type result in poorer outcomes compared with adenocarcinoma. Poor outcomes were also found in this study as 4 of 6 patients (66%) with mucinous adenocarcinoma and 2 patients with signet ring cell type died during the follow-up, and the median survival was only 24 months. Six of 19 patients developed peritoneal metastasis at the time of surgery, and 4 of them (66.6%) had mucinous adenocarcinoma and signet ring cell type. In contrast, the patients with adenocarcinoma had a mortality rate of 18.1% during the follow-up.
Another clinical feature of teenagers with sporadic CRC was their high pathological stage on diagnosis, with 52% of all patients having stage III or higher. Furthermore, their survival rate was low, resulting in only 2 patients surviving during the follow-up. Meanwhile, all of the 9 patients (47.2%) with stage II or lower survived during the follow-up. Therefore, this finding underscores the importance of early examination. However, teenagers usually do not undergo the clinical examination that adult patients undergo for early detection as CRC is so rare in teenagers, thereby resulting in the progression of CRC when a symptom-based diagnosis is made. As a result, CRC in teenagers is characterized by a low resection rate, poor prognosis, and high treatment failure compared with CRC in adults. These factors are coupled by the higher proportion of mucinous adenocarcinoma and signet ring cell type than that of adenocarcinoma, which produces a poor prognosis.
This study has limitations including the retrospective data analysis using a database and a small sample size (n= 19) despite the coverage period of 25 years. Given an extremely low incidence of CRC in teenagers, a multicenter study is imperative to collect more data and to provide further evidence.
Sporadic CRC is quite rare in teenagers. However, the incidence of histological subtypes associated with a poor prognosis tends to be higher than that in adults. In addition, their tumor stages were higher at the time of diagnosis, leading to an overall poor prognosis. Therefore, early detection at the premetastatic stage and subsequent radical surgical approaches, when possible, are important to improve prognosis.
Notes
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.